Insight
When Less Is More: A Guide to EHR De-Implementation
While burnout manifests in individuals, it originates in systems.
— CHRISTINE SINSKY, M.D.
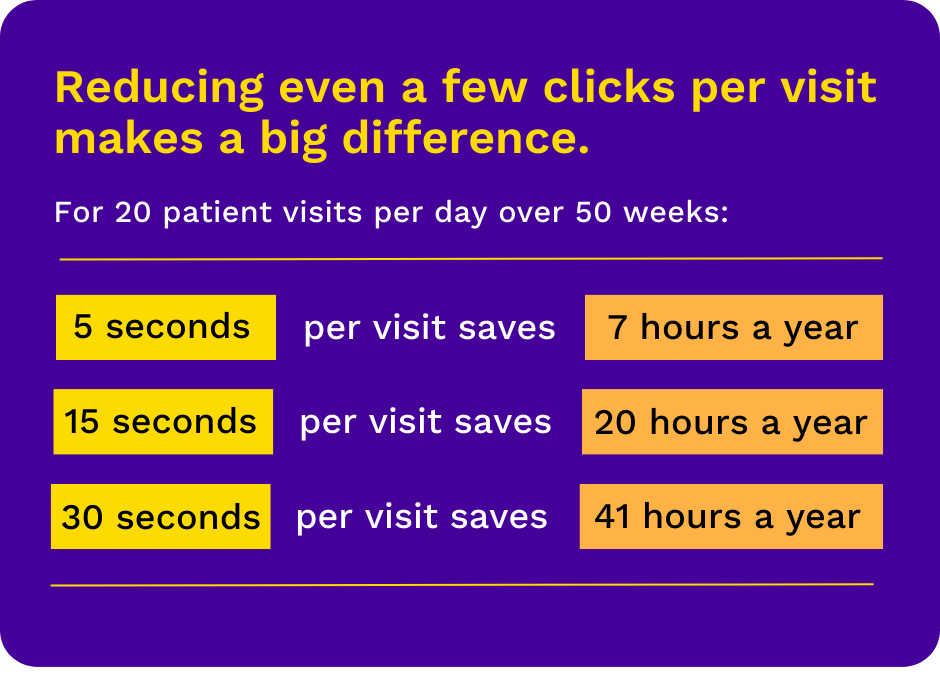
Is your EHR doing too much? With 44% of physicians reporting weekly signs of burnout, consider not only what your EHR should do–but also what it should stop doing. According to the American Medical Association, “de-implementing” unneeded tasks, clicks, notifications, and requests can save hours of clinical time each week, reducing administrative burden and saving valuable resources.
Involving clinical staff in EHR planning helps ensure that workflows align with physicians’ needs. But even well-designed EHR platforms can overburden physicians with unnecessary administrative tasks. Often, these inefficiencies are revealed after a system has been in use for some time. Over months and years, administrative tasks that were deemed essential are revealed to be unneeded.
Of course, physicians aren’t the only group burdened by inefficient or unnecessary EHR tasks. De-implementing unneeded clicks and processes helps support hospital staff, too. Unneeded clicks, requests, and requirements burden staff and slow down business operations, billing, laboratory services, and more.
Whether you’re planning a new EHR implementation or optimizing an existing system, consider reducing or eliminating these tasks to save clinical resources:
Alerts and Notifications
- Evaluate automatic alerts; keep only those shown to be necessary and beneficial
- Reduce inbox notifications, including multiple notifications for the same test
- Consider auto-release of normal and abnormal test results to the patient portal
- Eliminate notifications about reports sent to the person generating the report
Logins and Passwords
- Simplify login processes with options like bioidentification and RFID proximity identification
- Consider annual attestation instead of daily or every-login attestations as allowed by law
- Extend time before auto-logout to reduce the need for multiple logins within a single workflow
- Decrease password-related burdens by eliminating requirements for password revalidation and using password keeper programs
Notes and Orders
- Employ AI to help prioritize clinically relevant information in patient notes
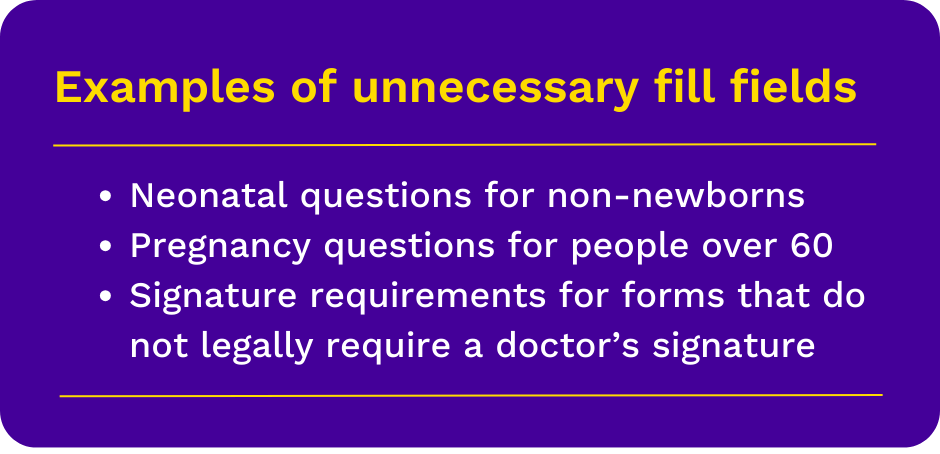
- Reduce clicks and hard-stops in ordering by reducing unnecessary fill fields
- Optimize order entry by auto-populating fields with data already in the EHR
- Allow verbal orders in low-risk and crisis situations as legally permitted
Compliance, Quality Assurance, and Learning
- Eliminate signature requirements for forms and orders that do not legally require a physician signature
- Consider eliminating “challenge questions” to electronically sign orders when the user is already logged in and actively using the EHR
- Evaluate annual trainings and remove those not required by law or lacking in evidence
- Perform condition screens no more frequently than recommended, and include a grace period to prevent wasting clinical resources